Did you hear? The latest version of the U.S. Dietary Guidelines, released earlier this year, has removed the recommended limit on cholesterol in the diet. Cholesterol is no longer a nutrient of concern. While most of us in the nutrition world have known for a long time that cholesterol in the diet does not affect risk for heart disease, we also know that it sometimes takes a while for policy to catch up with science.
So if cholesterol in food doesn’t cause high cholesterol, what does? While some might blame saturated fat and fructose (the latest fad), I’m going to dive in and explain to you a more in-depth, big picture view of cholesterol labs and your health.
The most important thing to know is that is that cholesterol isn’t this bad-for-you-you substance that it’s made out to be. Most people think, the lower your cholesterol, the better. If you could just get it down to zero you’d be in great shape! However, cholesterol is absolutely vital to the proper function of the human body. Your body makes cholesterol, regardless of your dietary intake, for good reason. If you had no cholesterol in your body, you would be dead! It plays an important role in digestion, Vitamin D status, hormone production and balance, and many other human body processes.
You also need to know that high cholesterol isn’t a diagnosis. It’s a symptom. Just because you have high cholesterol, doesn’t mean anything bad will happen! The words ‘high cholesterol’ inspire a feeling of dread as something akin to a death sentence. The mainstream narrative on cholesterol is that arteries are like pipes and cholesterol is like gunk. The pipes get clogged up with cholesterol, and then you have a heart attack. This is a powerful image, but it’s not accurate at all. First of all, at least half of all people who suffer a heart attack have normal cholesterol levels (1, 2). Second of all, after age 65, high cholesterol is associated with health and longevity (3). Third, plaques that “clog” arteries are actually made up of calcium and oxidized LDL particles (think rancid – more on that later), and they form under the artery wall (4). So get that vision of “clogged arteries” out of your head, and if you are a health professional, quit using those test tubes full of fat to scare people at health fairs!

Instead of looking at your high cholesterol labs with a sense of doom, let’s look at how cholesterol levels in the blood rise and when it becomes a problem.
One of the basic functions of cholesterol is to stabilize the mitochondria (the energy powerhouse of the cell), preventing their destruction by stress. Anytime you’re under a stressful situation, cholesterol rises as a protective response to the stressor. Yes, you read that right: cholesterol is a protective substance! Stress also lowers intracellular magnesium, which also causes cholesterol production to increase, since magnesium regulates the enzyme that makes cholesterol (5). Stress can be anything from psychological stress like that from jobs, family, money, etc., to physiological stress like skipping meals, not getting enough sleep, and eating poorly.
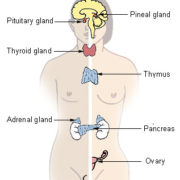
In youth and those with high metabolisms (good thyroid output AND uptake of thyroid hormone by cells), cholesterol is converted inside cells into pregnenolone, DHEA, testosterone, progesterone, and other important protective hormones. You cannot make these hormones without cholesterol!
Cells need two things to make the conversion: Vitamin A in its active form and thyroid hormone. As humans get older, their ability to convert beta carotene into active Vitamin A decreases, most Americans don’t eat much active Vitamin A in their diet, and metabolism decreases. In fact, up until about 40 years ago, high cholesterol was diagnostic of hypothyroidism, and routinely treated with supplemental thyroid hormones.
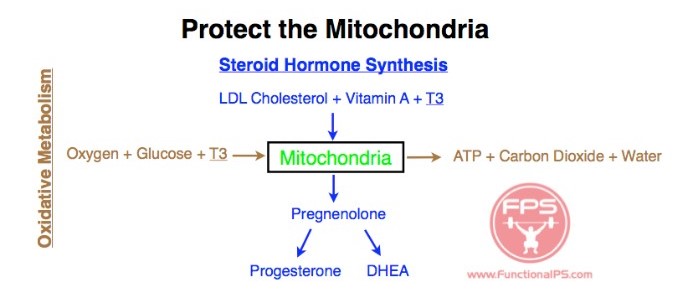
So high cholesterol is a problem because you’re not making youthful, protective hormones. But it’s also a problem because cholesterol oxidizes if it hangs around in the blood stream long enough, losing its protective functions. The cholesterol — or more accurately, the lipoproteins like LDL that are carrying cholesterol — get damaged by oxidation, and then the immune system’s response to that oxidative process is what causes the buildup of plaque and then ultimately the rupture of plaque and heart attack.
So the real question everyone should be asking when it comes to atherosclerosis and heart disease is: “what causes LDL to oxidize?”
There are three main ways oxidized cholesterol builds up in your bloodstream (6):
- eating commercially fried foods, such as fried chicken and French fries
- eating excess polyunsaturated fatty acids, which are found in vegetable oils, packaged food and restaurant food
- cigarette smoking
Your doctor, and most dietitians for that matter, will tell you that polyunsaturated fats from refined vegetable oils, margarine, nuts, seeds, and other plant foods lower your cholesterol. And they’re right! But given what you just learned about cholesterol, do you really think lowering your body’s protective production of cholesterol is a good idea?! Within this framework, the effect of polyunsaturated fats is the same as the effect from statins, which come along with nasty side effects. I hope after reading this, you’ll start to understand physiologically why statins have the side effects they do, and why they’re not very helpful for most people (7).
A note about Paleo diets and fructose. Paleo bloggers and gurus have been pretty hard on fructose recently, blaming carbs and sugar for raising cholesterol. “Quit sugar and watch your cholesterol plummet!” Yup, also watch your libido and energy tank from lack of fuel for the liver and brain. Don’t fall for the low-carb trap when trying to lower your cholesterol. Fructose has pretty much been absolved of any wrongdoing in my book (8, 9).
If you have high cholesterol and your doctor is concerned, here is what I would advise:
- Ask your doctor for a cholesterol particle size test (LDL-P). Small LDL particles are more likely to oxidize and form plaques under the artery walls (10).
- Know your calcium status. One of my favorite things about Mineral Analysis, is the crucial information on tissue calcium it gives me. Coronary calcium scans will also give you good information about your tissue calcium buildup (4).
- Have your thyroid status checked. This involves more than a TSH test! Blood lab work, including TSH, will tell you if your thyroid gland is producing enough thyroid hormone, but tells you nothing about your cells’ ability to use it. Broda Barnes was an American physician who was able to reduce heart disease incidence in his almost 2,000 patients by 90 percent. He used basal body temperature first thing in the morning as an indicator for thyroid uptake. Anything less than 97.8 degrees was considered functionally hypothyroid (11).
If you want to lower your cholesterol in a physiologically-sound way, that ensures proper body function for years to come:
- Make sure your diet has plenty of sources of active Vitamin A. Eggs, liver, and grass-fed dairy are examples. Hmmm, imagine that….all potent sources of cholesterol! It’s like nature has a plan or something…
- Make sure your diet has plenty of Vitamin K2, active Vitamin K. K2 is a calcium director and can remove calcium buildup from the arteries (12). It’s found in, again, eggs, liver, and grass-fed dairy. This is sounding more and more like a French diet. It’s not genes or the wine protecting them from heart disease (13).
- Eat plenty of potassium-rich foods, like fruits and vegetables (14). You are likely not eating enough.
- Eat more magnesium and supplement if needed. Cooked dark leafy greens and organic dark chocolate are good sources. Magnesium is also absorbed topically through the skin.
- Destress!
- Focus on all the things that improve thyroid uptake by cells: get enough calories, protein, carbohydrates, potassium and other minerals, good estrogen metabolism, and good liver function – AKA all the things I work on with clients!
- https://www.uclahealth.org/most-heart-attack-patients-cholesterol-levels-did-not-indicate-cardiac-risk
- https://www.cnn.com/2021/04/23/health/cholesterol-versus-saturated-fat-wellness/index.html
- https://www.sciencedaily.com/releases/2016/06/160627095006.htm
- http://jeffreydachmd.com/how-to-reverse-heart-disease-with-the-coronary-calcium-score/
- http://www.ncbi.nlm.nih.gov/pubmed/16272615
- https://universityhealthnews.com/daily/heart-health/oxidized-cholesterol-vegetable-oils-identified-as-the-main-cause-of-heart-disease/
- http://www.thennt.com/nnt/statins-for-heart-disease-prevention-without-prior-heart-disease/
- http://www.alanaragonblog.com/2010/01/29/the-bitter-truth-about-fructose-alarmism/
- http://www.ncbi.nlm.nih.gov/pubmed/20047139
- https://labtestsonline.org/understanding/analytes/lipoprotein-subfractions/tab/test/
- https://www.amazon.com/Hypothyroidism-Unsuspected-Illness-Broda-Barnes/dp/069001029X/ref=sr_1_fkmr1_3?ie=UTF8&qid=1469410638&sr=8-3-fkmr1&keywords=hypothyroid+broda
- http://www.todaysdietitian.com/newarchives/060113p54.shtml
- http://www.drdeborahmd.com/healing-multiplied-k2-super-supplement
- http://www.ncbi.nlm.nih.gov/pubmed/2632721